It’s hard not to have COVID on the brain in today’s world – it seems like every conversation ends up on the topic! A recent study completed at Columbia explored the effect of COVID in the brain, by collecting brain samples from the mesial temporal cortex, a brain region implicated in Alzheimer’s disease and responsible for memory, and the cerebellum, a brain region responsible for coordination of movement and balance. Different cellular markers that indicate inflammation and protein build-up in the brain were measured in 10 patients who had passed away from COVID-19 and were compared to brains of those who did not have COVID-19 at the time of death. From this, the researchers were able to infer how COVID-19 infection may alter the brain, potentially causing the neurological symptoms in some COVID patients.
COVID-19 infection can lead to respiratory, cardiac, and neurological symptoms. About one in three COVID patients experience neurological symptoms including loss of taste (hypogeusia), loss of smell (hyposmia), headache, disturbed consciousness, and tingling sensations in their limbs (paresthesia). The exact reason why these neurological symptoms occur is not well understood. In a recent publication, Dr. Steve Reiken and colleagues from the Department of Physiology and Cellular Biophysics at Columbia University Vagelos College of Physicians and Surgeons explore how factors associated with COVID infection, like inflammation, led to these neurological symptoms.
SARS-CoV-2, the virus that causes COVID-19, enters the body through the airways. The spike proteins on the surface of SARS-CoV-2 virus facilitate the entry into cells through the angiotensin converting enzyme 2 (ACE2) receptor. This leads to inflammation in the lungs and other organs. ACE2 receptors are downregulated during COVID infection, a pattern which has been tied to an upregulation of inflammatory marker transforming growth factor-𝛃 (TFG-𝛃) in other disease models including cancer. Lower ACE2 activity has also been tied to greater concentrations of Alzheimer’s disease (AD) related proteins amyloid-𝛃 (A𝛃) and phosphorylated tau. Perhaps the entry-point of the SARS-CoV-2 virus activates inflammation pathways that can affect the brain similar to the way it is affected in AD, and might cause the neurological issues that sometimes come with COVID infection.
In the study, inflammation markers that represent TFG-𝛃 levels were measured in the brain samples of COVID patients and were compared to non-patients. Each of these measures were higher in brain samples of COVID patients, suggesting that COVID infection contributed to more inflammation in the brain.
Inflammation may have downstream effects that can impact the function of healthy tissues. For example, the highly-regulated use of the calcium ion (Ca2+), which is a key player in cell-to-cell communication, can become impaired in conditions of inflammation. Specifically, the ryanodine receptor (RyR) is an ion channel protein which is responsible for Ca2+ release. When in an open configuration, Ca2+ can flow freely through the channel. To stop Ca2+ flow, helper proteins interact with the RyR to stabilize the closed configuration of the channel. Previous studies have suggested that these helper proteins are downregulated in inflammation, which means that the RyR is more likely to be unstable, resulting in excess Ca2+ flow, or a Ca2+ leak. Ca2+ leaks have been thought to contribute to a number of diseases, including the development of tau pathology in AD.
In Dr. Reiken and colleagues’ study, indicators of typically functioning RyR were measured in the brain samples of COVID patients and non-patients. These measures included the amount of RyR channel in the open configuration (which means a lot of free flowing Ca2+) and the concentration of the helper proteins that helps the RyR remain stable in the closed configuration. The researchers found that there were less helper proteins in the COVID brains compared to the non-COVID brains. Additionally, more of the RyR channels were in an open configuration in the COVID brains compared to non-COVID brains. This means that Ca2+ leaks were more likely to happen in the brains of those infected with COVID-19.
In addition to cellular markers of inflammation and Ca2+ leaks, Dr. Reiken and colleagues also investigated levels of AD-related proteins A𝛃 and tau aggregation in the brains of control subjects and COVID patients. For A𝛃, relevant protein levels were similar between COVID patients and controls, suggesting that COVID does not cause the collection of A𝛃 in the brain. However, the concentration of phosphorylated tau, another protein that is highly implicated in AD pathology, was higher in the temporal lobe and cerebellum regions in COVID patients compared to control subjects.
To take this one step further, the researchers treated the COVID patients’ brain samples with Rycal ARM210, a drug that is currently in clinical trials for other applications at the NIH (NCT04141670) and helps to reduce Ca2+ leak. With ARM210, helper protein levels in the COVID brain samples increased from the original levels in the COVID brain samples that were not treated with the drug. Additionally, the amount of RyR in the open configuration decreased in the COVID brain samples with ARM210, compared to the un-treated samples. Thus, treatment with this drug may combat Ca2+ leak in brain tissue. If unstable RyR leads to the Ca2+ leak, and Ca2+ leak can promote tau phosphorylation and build up in the brain, then using the Rycal drug ARM210 to target and limit Ca2+ release may potentially be a way to treat of these brain abnormalities in COVID-19 and possibly minimize neurological symptoms.
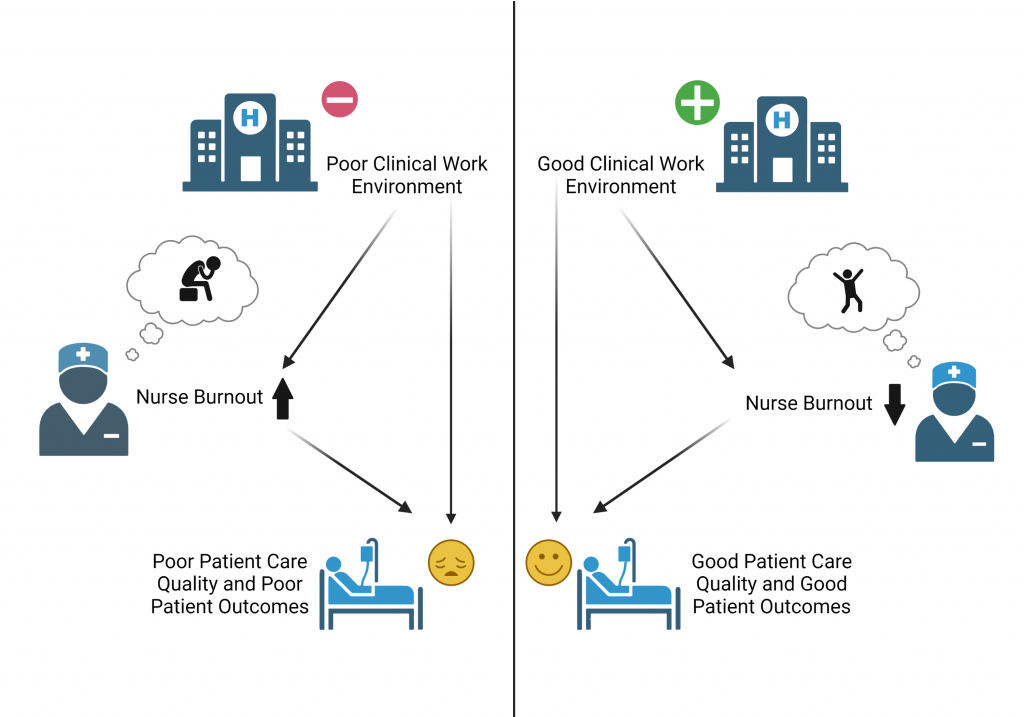
Given these results, the authors propose a mechanism by which infection with the SARS-CoV-2 virus may lead to protein aggregation similar to tau deposition in AD. An adaptation of the proposed mechanism is shown in the Figure below.

Figure 1 (above): Proposed mechanism for neurological symptoms of COVID-19 infection. Adapted from Reiken et al., 2022. Created with BioRender.com.
Though this is a very exciting study exploring the neurobiology in COVID brains, there are some additional things to consider. Firstly, while inflammatory markers were elevated in the brains of COVID patients, SARS-CoV-2 virus particles were not detectable in the brain. This suggests that these effects are caused by systemic factors, and are not localized to cells that are infected with SARS-CoV-2. Additionally, in terms of the AD-related proteins, elevated phosphorylated tau protein was detected in the mesial temporal cortex and the cerebellum of COVID patients compared to controls. In AD, tau protein collects in the medial temporal cortex early in disease progression, but does not collect in the cerebellum. This, in addition to the lack of A𝛃 aggregation in the COVID patients’ brain samples, is a marked difference between the pathology of the brain in AD and in COVID. However, distribution and amount of tau protein in AD is linked to cognitive abilities, so perhaps the collection of tau in the brain of COVID contributes to cognitive symptoms like “brain fog”. The current study used brain samples from 10 COVID patients, but did not collect cerebrospinal fluid samples or use animal models to validate these findings yet. Future work that addresses these limitations and further questions may help us fully understand the role of COVID in the brain, and may help with treatments for those who are struggling with prolonged neurological symptoms of COVID.
–
Dr. Reiken, the first author of this work, is an Assistant Professor at Columbia University Department of Physiology. Dr. Dridi, a Postdoc Fellow at Columbia, and Dr. Liu, a Postdoc Research Scientist at Columbia, also contributed to this work. Find the original research article here.
–
Reference:
Reiken, S, Sittenfeld, L, Dridi, H, Liu, Y, Liu, X, Marks, AR. Alzheimer’s-like signaling in brains of COVID-19 patients. Alzheimer’s Dement. 2022; 1- 11. https://doi.org/10.1002/alz.12558