Precious Esie, Lisa Bates, and colleagues recently published their work examining the relationship between the severity of intimate partner violence (IPV) and the risk for a major depressive episode (MDE) in the journal Social Science and Medicine –Population Health. The authors applied a novel approach to measuring IPV by operationalizing IPV as the frequency of various acts of physical, psychological, and sexual IPV separately, as well as experiencing injury due to physical or sexual IPV — in contrast to using standard dichotomous indicators. The study population consisted of women who were between 16-37 years old and were married for 4-12 years to their current husband. Experiences of IPV were recent, occurring within 10 months (on average) prior to interviews.
The figure below illustrates the ubiquity and multi-dimensionality of IPV in rural Bangladesh. Nearly 83% of women experienced some form of recent IPV, and nearly all women who experienced physical or sexual IPV also experienced psychological IPV.
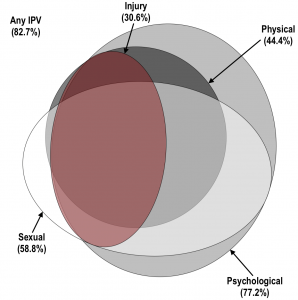
Euler diagram illustrating the prevalence and co-occurrence of physical, psychological, and sexual IPV, as well as injury due to physical or sexual IPV
The authors found that incorporating IPV severity consistently revealed a substantially elevated risk of recent MDE for all forms of IPV. Alternatively, the standard dichotomous measures of IPV appeared to underestimate the elevated risk of MDE associated with IPV exposure. For example, in the figure below, although the most severe exposure to sexual IPV was significantly associated with a 65% increased risk for MDE, the corresponding dichotomous measure of sexual IPV (experiencing at least one act versus none) indicated no significant increase for MDE (RR=1.15; 95% CI: 0.90–1.48). This suggests dichotomous indicators of IPV may fail to reveal an association with MDE, but also obscure the much more elevated risks associated with severe levels of IPV exposure.
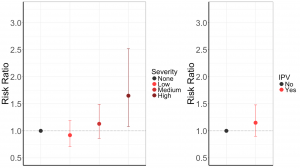
Risk ratio for sexual IPV severity (left) and as a dichotomous indicator (right).
Notably, the authors also found that for all forms of IPV, the lowest levels of violence severity were not associated with an elevated risk for MDE, relative to no IPV. These results deviate from what has been observed in high-income countries, where as little as one episode of IPV may be associated with more than twice the risk for depression (e.g. Miszkurka et al., 2012). In sum, the use of dichotomous measures, at least in high-prevalence settings such as rural Bangladesh, may mask important nuances in the relationship between IPV and depression and more work is necessary to help explain the IPV-depression gradient.
References:
Miszkurka, M., Zunzunegui, M.V., & Goulet, L. (2012). Immigrant status, antenatal depressive symptoms, and frequency and source of violence: what’s the relationship? Archives of Women’s Mental Health, 15, 387-396.